 |
 |
- Search
| Ann Pediatr Endocrinol Metab > Volume 27(1); 2022 > Article |
|
Abstract
The Committee on Pediatric Bone Health of the Korean Society of Pediatric Endocrinology has newly developed evidence-based clinical practice guidelines for optimizing bone health in Korean children and adolescents. These guidelines present recommendations based on the Grading of Recommendations, which includes the quality of evidence. In the absence of sufficient evidence, conclusions were based on expert opinion. These guidelines include processes of bone acquisition, definition, and evaluation of low bone mineral density (BMD), causes of osteoporosis, methods for optimizing bone health, and pharmacological treatments for enhancing BMD in children and adolescents. While these guidelines provide current evidence-based recommendations, further research is required to strengthen these guidelines.
The Committee on Pediatric Bone Health of the Korean Society of Pediatric Endocrinology has newly developed evidence-based clinical practice guidelines for optimizing bone health in Korean children and adolescents. These guidelines include processes of bone acquisition, definition, and evaluation of low bone mineral density (BMD), causes of osteoporosis, methods for optimizing bone health, and pharmacological treatments for enhancing BMD in children and adolescents.
Osteoporosis was previously thought to be a disease exclusive to older adults. However, it is now increasingly recognized in younger adults due, in part, to the longer survival of chronically ill children. Children with osteoporosis are at a high risk of skeletal morbidity not only during youth, but also in adult life [1]. Bone mass attained in early life is thought to be the most important modifiable determinant of lifelong skeletal health [2]. In this context, the Committee on Pediatric Bone Health of the Korean Society of Pediatric Endocrinology recently developed evidence-based clinical practice guidelines for optimizing bone health in Korean children and adolescents. Recommendations were determined according to the quality of evidence graded by the steering committee on quality improvement and management in the American Academy of Pediatrics [3].
This guideline comprises the physiological processes of bone acquisition, definition, and evaluation of low bone mineral density (BMD), causes of osteoporosis, conservative management for optimizing bone health, and pharmacological treatments for enhancing BMD in children and adolescents.
Bone is a living structure comprising a matrix of collagen, hydroxyapatite crystals, and noncollagenous proteins. The matrix becomes mineralized with deposits of calcium and phosphate, which confer strength to the structure [1].
Bone mineral deposition begins in utero, and bone mineral content increases 40-fold from birth to adulthood. BMD of the lumbar spine (BMDLS) showed the greatest increase from the age of 11 to 13 years in girls and from 12 to 14 years in boys. BMD of the total body less head (BMDTBLH) shows a relatively modest increase from the age of 10 to 15 years in girls and from 10 to 18 years in boys [4,5]. In Korea, peak bone mass is achieved at approximately 19 and 21 years of age in girls and boys, respectively [6,7].
There are numerous factors that affect bone mineral deposition and bone mass formation. These are largely divided into 2 groups: nonmodifiable factors including genetics, sex, and ethnicity and modifiable factors including nutrition, exercise, lifestyle, body weight and composition, and hormonal status [8].
BMD in children and adolescents is most commonly assessed with dual-energy x-ray absorptiometry (DXA) because it is less time-consuming and more precise and widely available, safer, and less costly than other options [9]. The posteroanterior lumbar spine and total body less head are the preferred skeletal sites for BMD measurement in most pediatric patients, while other sites are recommended only for specific cases [9]. BMDLS measurement is a feasible and reproducible method, especially for infants and young children aged 0–5 years. BMDTBLH measurement can be used for children aged 3 years and older [9]. The standard methods of BMD evaluation in children and adolescents are performed using BMD z-score calculations according to comparisons with reference data in children of each age, sex, pubertal stage, and ethnicity [6,7,9]. In children with short stature or growth delay, BMDLS should be adjusted with bone mineral apparent density or height z-score and BMDTBLH with the height z-score [9].
Low BMD is the preferred term for DXA reports in children when the BMD z-score is less than or equal to -2.0 standard deviation (SD) [9]. Osteoporosis in children is defined as the presence of ≥1 vertebral compression fracture in the absence of local disease or high-energy trauma or the presence of both a clinically significant fracture history and a BMD z-score of -2.0 or lower. A clinically significant fracture history includes at least one of the following: (1) ≥2 long bone fractures by the age of 10 years and (2) ≥3 long bone fractures at any age up to 19 years [9].
There are primary and secondary causes of reduced bone mass and increased fracture risk (Table 1). Primary osteoporosis occurs due to intrinsic skeletal defects originating from genetic or idiopathic causes, while secondary osteoporosis results from chronic systemic illnesses in children due to either the effects of the disease process on the skeleton or from treatment [8,10,11].
Osteogenesis imperfecta is a rare genetic disorder with an incidence of approximately 1/25,000. Clinical manifestations include low bone mass, frequent fractures, bone deformity, short stature, wormian bones, blue sclerae, hypermobility of joints, dentinogenesis imperfecta, and deafness. There are 5 types of osteogenesis imperfecta according to clinical severity. Type 1 is the least severe and nondeforming; type 2 is lethal in the perinatal period because of respiratory insufficiency due to multiple rib fractures; type 3 is associated with limb deformities and is progressively deforming; type 4 has an intermediate phenotype between types 1 and 3; and type 5 has a phenotype similar to that of type 4 but is associated with calcification of interosseous membranes and hypertrophic callus formation at healing fracture sites. The most common mutations in all types are found in COL1A1 and COL1A2, but novel mutations in other genes have been found (Table 2) [10].
Idiopathic juvenile osteoporosis is a disease of unknown etiology that is considered genetically heterogeneous in origin. The clinical manifestations include bone pain and fractures with minimal trauma in girls or boys aged 8–12 years. Symptom severity tends to abate spontaneously with variable residual manifestations [10,12]. Differential diagnosis of osteogenesis imperfecta and idiopathic juvenile osteoporosis is shown in Table 3.
Osteoporosis-pseudoglioma syndrome is a congenital or infantile-onset disease. Its clinical manifestations include severe visual impairment, bone fragility, ligamentous laxity, hypotonia, and cognitive impairment. It is transmitted as an autosomal recessive trait and is associated with several types of mutations in LRP5 [10].
Hypogonadism, growth hormone (GH) deficiency, hyperthy roidism or hypothyroidism, hyperparathyroidism, diabetes mellitus (DM), and Cushing syndrome are associated with low bone mass [8,10,11]. Hypogonadism is associated with decreases in cortical width, trabecular number, and osteoid and mineralization activity because of the decreased lifespan of osteoblasts and osteocytes but increased lifespan of osteoclasts, histomorphometrically [13] GH deficiency is associated with decreases in osteoblast differentiation and proliferation, osteoblast synthesis of insulin-like growth factor-I (IGF-I), insulin-like growth factor binding protein-3, osteocalcin, bone-specific alkaline phosphatase, procollagen type I, and osteoprotegerin [14,15].
Thyroid disorders also lead to secondary osteoporosis in children. In hyperthyroidism, rates of cartilage maturation, bone turnover, and osteoclastogenic effects increase [16]. In hypothyroidism, cartilage maturation and endochondral bone formation decrease. Additionally, thyroid hormone deficiency in early life delays the development of epiphyseal centers of ossification [16]. In hyperparathyroidism, excess parathyroid hormone induces the production of receptor activator for nuclear factor κB ligand (RANKL) and inhibits the production of osteoprotegerin, increasing osteoclastogenesis and bone resorption [11].
In DM, hyperglycemia is related to accumulation of glycated proteins, which impairs differentiation of mesenchymal stem cells into chondrocytes and osteoblasts with decreased synthesis of osteocalcin [17]. Finally, in Cushing syndrome, glucocorticoid excess is directly associated with inhibition of osteoblastogenesis and promotion of osteoblast and osteocyte apoptosis. Further, the excess glucocorticoid indirectly impairs bone accretion by inhibiting secretion of IGF-I and intestinal calcium absorption [18-20].
Anorexia nervosa and female athlete triad are examples of both nutrition- and hormone-induced bone loss that can lead to early-onset osteoporosis [8].
Numerous medications such as glucocorticoids, anticonvul sants, chemotherapeutic agents, immunosuppressive agents, heparin, proton pump inhibitors, and selective serotonin reuptake inhibitors can increase the risk of low bone mass [8]. In children, studies have reported that use of oral glucocorticoids for more than 3 months reduced bone density and increased the risk of spinal compression fractures. Therefore, it is recommended that glucocorticoids be used in low doses every other day rather than every day, while maintaining calcium and vitamin D concentrations in the normal range. As short-term administration or inhaled formulations of corticosteroid can also affect bone density [1], it is difficult to recommend safe doses and durations [19].
In pediatric patients with primary bone disease or those at risk of secondary bone disease, DXA should be performed when the patient might benefit from interventions to decrease the risk of clinically significant fracture. If follow-up DXA is indicated, the minimum interval between scans should be 6–12 months [9]. The evaluation processes according to risk of osteoporosis are shown in Fig. 1.
Modifiable determinants of bone mass include nutrition, exercise, lifestyle, body weight, lean body mass, and hormonal status. These conditions should be adequately maintained to optimize bone health [8].
Many studies have reported that calcium and vitamin D supplementation is helpful in increasing bone mass and BMD in children. These nutritional elements should be supplemented using food rather than medicine in healthy children [34-37]. Many types of foods are good dietary sources of calcium and vitamin D. Human milk or infant formula is the primary source of calcium for healthy infants in the first year, and milk and other dairy products are the major sources of calcium after the first year of life. Other dietary sources include green leafy vegetables, legumes, nuts, cereal, and fruit juices. The bioavailability of calcium from vegetables is generally high but is reduced by binding with oxalate in spinach, collard greens, and beans and with phytate in whole bran cereals. Natural dietary sources of vitamin D include cod liver oil, salmon, sardines, tuna, and fortified foods. Exposure to ultraviolet B radiation from sunlight is the major source of vitamin D production [8]. The recommended daily allowance and upper limit of calcium and vitamin D are shown in Table 4 [8,36-39]. If calcium or vitamin D deficiency causes low BMD, it should be administered at a therapeutic dosage (Table 5) [8,40]. Several types of vitamin D prescriptions are available including ergocalciferol (vitamin D2), cholecalciferol (vitamin D3), alphacalcidol (1α-hydroxyvitamin D3), and calcitriol (1,25-dihydroxyvitamin D3). Vitamin D3, an active form of vitamin D, is frequently used in children with vitamin D deficiencies. Alphacalcidol or calcitriol is used in children with renal diseases [8].
Ingestion of adequate amounts of calories, proteins, and vegetables or fruits containing high vitamin C, vitamin K, potassium, magnesium, copper, and manganese contents is also needed to maintain bone health in children [41]. The prescription forms of calcium are calcium carbonate (40% elemental calcium), calcium citrate (21% elemental calcium), calcium lactate (13% elemental calcium), and calcium glutamate (9% elemental calcium). Calcium carbonate should be taken with meals to promote absorption, but calcium citrate can be taken on an empty stomach. The adverse effects of consuming excessive calcium are dyspepsia, constipation, urinary stones, and hypercalcemia, especially when taken with vitamin D [8].
Mechanical forces applied to the skeleton increase bone formation, and weight-bearing exercises improve bone mineral deposition [42-45]. High-impact and low-frequency exercises such as jumping, skipping, and hopping for 10 minutes 3 times per week increases the BMD of the femoral neck in healthy children [46]. Weight-bearing exercises such as walking, jogging, jumping, and dancing are better than non-weight-bearing exercises such as swimming or bicycle riding [45,46]. However, excessive high-impact and prolonged exercises can increase fracture risk; therefore, children who want to participate in these sports should cross-train with low-impact activities [47].
Estrogen, testosterone, GH, and IGF-I c an promote bone formation, but excess glucocorticoid increases bone resorption [8,10,11]. Therefore, bone mineral depositions in children with endocrine disorders, such as hypogonadism, Turner syndrome, GH deficiency, and Cushing syndrome, should be carefully investigated and adequately maintained.
Bi sphosphonate s i n h ibit oste o cl a st - me d i ate d b one resorption and prevent osteoblast or osteocyte apoptosis. These medications have been used in children with osteogenesis imperfecta, diseases treated with corticosteroids, cerebral palsy, and connective tissue diseases. Bisphosphonates have been reported to increase BMD and decrease pain and fracture in children with these diseases. However, their use in children remains controversial because of long half-lives and potential adverse effects [49]. The various prescription forms of bisphosphonates are shown in Table 6.
Bisphosphonates are commonly prescribed for individuals with osteogenesis imperfecta. Many reports have demonstrated that oral or intravenous bisphosphonates increase BMD in children and adults with this condition [50,51]. Most patients with idiopathic juvenile osteoporosis tend to remit spontaneously, but if there is a possibility of permanent deformity after vertebral or long bone fracture, bisphosphonate treatment should be considered [52].
Bisphosphonates should be used in children with recurrent extremity fractures, symptomatic vertebral collapse, and severe bone pain caused by other clinical conditions but should not be used to treat asymptomatic reduction in bone mass in children [53]. In addition, sufficient nutrition including calcium/vitamin D, adequate body weight, physical activity within the possible range, and supplementation in cases of hormone deficiencies should be prioritized over bisphosphonate treatment [54]. Bisphosphonates have been reported to be effective for pediatric patients presenting with secondary osteoporosis with cerebral palsy, juvenile idiopathic arthritis, renal transplantation, renal disease with chronic steroid therapy, Crohn disease, Duchenne muscular dystrophy, leukemia or lymphoma with chemotherapy, or chronic graft-versus-host disease [55-64].
Although guideline consensus for bisphosphonate forms, dosage, treatment duration, and interval of administration is needed in children, pamidronate is often used in young children, followed by switching to zoledronate in older patients with moderate-to-severe disease [54]. Pamidronate doses vary from 9 to 12 mg/kg/yr in 4 to 6 divided doses, and zoledronate is initiated at 0.1 mg/kg/yr in 2 divided doses. The starting doses for pamidronate and zoledronate are usually recommended to be reduced to 0.5 mg/kg and 0.0125 or 0.025 mg/kg respectively, to minimize acute-phase reactions and hypocalcemia. Maintenance therapy at reduced doses is determined by a combination of fracture history, bone pain, BMD, and growth. The maintenance dosages for pamidronate and zoledronate are 3.0 and 0.025 mg/kg/yr, respectively, administered in 2 divided doses [54]. The typical treatment approaches for children with primary and secondary osteoporosis are shown in Fig. 2.
Contraindications for bisphosphonate therapy include pregnancy, severe renal disease, and active rickets. Reduced renal function is a relative contraindication because approximately 40%–60% of the dose is distributed to the bone; the remainder is excreted unaltered in the urine, with no substantial metabolism [65,66]. The acute adverse effects of bisphosphonate treatment in pediatric patients are flu-like symptoms and hypocalcemia, with possible long-term effects of delayed bone healing, osteopetrosis, and gastroesophageal reflux. The potential side effects are atypical femoral fractures, osteonecrosis of the jaw, orbital inflammation, growth impairment, and teratogenicity [65,66]. Therefore, clinical, biochemical, and imaging assessments must be performed [49,54]. General clinical examination with growth and nutritional evaluation, dental and eye examination, complete blood cell count, electrolytes, alkaline phosphatase, bone turnover markers, liver function test, renal function test, serum vitamin D and parathyroid hormone levels, urine analysis, urinary calcium excretion, radiography of the wrist and knee, and BMD should be included in the assessments [49,54].
Several new drugs, such as teriparatide (recombinant human parathyroid hormone), strontium ranelate, and denosumab (monoclonal anti-RANKL antibody), increase bone formation and decrease bone resorption. However, reports on the effect and safety of these medications in children are insufficient [10,11,67].
Bone mineral deposition shows the highest increase during the pubertal period in girls and boys and can be a major determinant of BMD in later life. Therefore, modifiable determinants of bone mass, including nutrition, exercise, lifestyle, body weight, lean body mass, and hormonal status should be adequately maintained to optimize bone health in children and adolescents.
The definition of osteoporosis in children is different from that in adults. In pediatric patients with primary or secondary osteoporosis, underlying conditions should be treated first, and then conservative and pharmacologic therapies should be considered.
Notes
ACKNOWLEDGMENTS
The Authors greatly appreciate the help from Pf. Choong Ho Shin (Past President of The Korean Society of Pediatric Endocrinology) and Pf. Ho Yeon Chung (Past Chairman of The Korean Society for Bone and Mineral Research) in organizing the committee for these guidelines. Further, Pf. Deog Yoon Kim (Past Chairman of The Korean Society for Bone and Mineral Research), Pf. Yumie Rhee (Secretary General, The Korean Society for Bone and Mineral Research), Pf. Seong Bin Hong (Director, Committee of Legislation and Ethics, The Korean Society for Bone and Mineral Research), Hye Ran Yang (Director of the External Cooperation Committee, The Korean Society of Pediatric Gastroenterology, Hepatology, and Nutrition), Ara Ko (The Korean Child Neurology Society), Joo Hoon Lee (Director of the Education and Training Committee, Korean Society of Pediatric Nephrology), Jun Ah Lee (Director of the Committee of Insurance, The Korean Society of Pediatric Hematology- Oncology) provided significant counsel for these guidelines.
Also, we would like to thank Eworldediting (www.eworldediting.com) & Editage (www.editage.co.kr)for English language editing.
Fig. 1.
The algorithm for assessment of bone health in children and adolescents. BUN, blood urea nitrogen; Cr, creatinine; PTH, parathyroid hormone; DXA, dual-energy x-ray absorptiometry; BMD, bone mineral density; Tx, treatment.

Fig. 2.
(A) Bisphosphonate treatment in patients with osteogenesis imperfecta (OI). (B) Bisphosphonate treatment in patients with secondary osteoporosis. DXA, dualenergy x-ray absorptiometry; BMD, bone mineral density; Tx, treatment. *Pamidronate 9 mg/kg/yr, 4–6 divided doses or zoledronate 0.1 mg/kg/yr, 2 divided doses. †Initial Tx of bisphosphonate, pamidronate 9 mg/kg/year, 4-6 divided doses or zoledronate 0.1 mg/kg/year, 2 divided doses. ‡Maintenance Tx, pamidronate 3 mg/kg/yr in 2 divided doses or zoledronate 0.025 mg/kg annually. Modified from Simm et al. J Paediatr Child Health 2018;54:223-33, with permission of Paediatrics and Child Health Division (The Royal Australasian College of Physicians) [54].
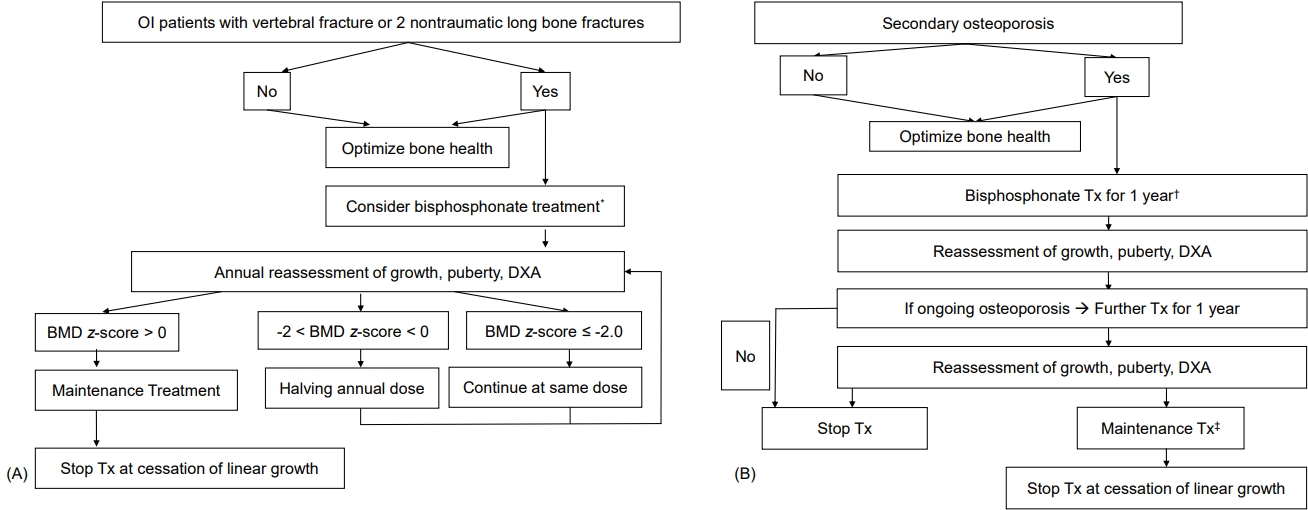
Table 1.
Causes of osteoporosis in children and adolescents
Table 2.
Types of osteogenesis imperfecta
Table 3.
Differential diagnosis between osteogenesis imperfecta and idiopathic juvenile osteoporosis
Table 4.
Dietary reference intake of calcium and vitamin D according to age
RDA, recommended daily allowance; UL, upper limit; M, male; F, female.
Adapted from The Korean Nutrition Society. 2020 Dietary Reference Intakes for Koreans. [38]
Table 5.
Treatment of Vitamin D deficiency according to Guidelines
Adapted from Holick et al. J Clin Endocrinol Metab 2011;96:1911-30. [40]
Table 6.
Name, route of administration, dose, and relative potency of bisphosphonates
PO, per os; IV, intravenous.
Adapted from Baroncelli and Bertelloni. Horm Res Paediatr 2014;82:290-302. [49]
References
2. Heaney RP, Abrams S, Dawson-Hughes B, Looker A, Marcus R, Matkovic V, et al. Peak bone mass. Osteoporos Int 2000;11:985–1009.


3. American Academy of Pediatrics Steering Committee on Quality Improvement and Management. Classifying recommendations for clinical practice guidelines. Pediatrics 2004;114:874–7.



4. Boot AM, de Ridder MA, van der Sluis IM, van Slobbe I, Krenning EP, Keizer-Schrama SM. Peak bone mineral density, lean body mass and fractures. Bone 2010;46:336–41.


5. Berger C, Goltzman D, Langsetmo L, Joseph L, Jackson S, Kreiger N, et al. Peak bone mass from longitudinal data: implications for the prevalence, pathophysiology, and diagnosis of osteoporosis. J Bone Miner Res 2010;25:1948–57.


6. Lim JS, Hwang JS, Lee JA, Kim DH, Park KD, Cheon GJ, et al. Bone mineral density according to age, bone age, and pubertal stages in Korean children and adolescents. J Clin Densitom 2010;13:68–76.


7. Yi KH, Hwang JS, Kim EY, Lee JA, Kim DH, Lim JS. Reference values for bone mineral density according to age with body size adjustment in Korean children and adolescents. J Bone Miner Metab 2014;32:281–9.


8. Golden NH, Abrams SA, Committee on Nutrition. Optimizing bone health in children and adolescents. Pediatrics 2014;134:e1229–43.


9. Bishop N, Arundel P, Clark E, Dimitri P, Farr J, Jones G, et al. Fracture prediction and the definition of osteoporosis in children and adolescents: the ISCD 2013 Pediatric Official Positions. J Clin Densitom 2014;17:275–80.


10. Root AW, Levine MA. Disorders of mineral metabolism II. Abnormalities of mineral homeostasis in the newborn, infant, child and adolescent. Sperling MAet al., editors. Pediatric endocrinology. 5th ed. Philadelphia (PA): Elsevier. 2021;pp 705–813.
11. De Paula F, Black DM, Rosen CJ. Osteoporosis: basic and clinical aspects. Melmed S, Auchus RJ, Goldfine AB, Koennig RJ, Rosen CJet al., editors. William's textbook of endocrinology. 14th ed. Philadelphia (PA): Elsevier. 2020;pp 1256–97.
12. Imerci A, Canbek U, Haghari S, Surer L, Kocak M. Idiopathic juvenile osteoporosis: a case report and review of the literature. Int J Surg Case Rep 2015;9:127–9.



13. Drake MT, Khosla S. Role of sex steroids in the pathogenesis of osteoporosis. Rosen CJ. Primer on the metabolic bone diseases and disorders of mineral metabolism. 7th ed. Washington DC: The American Society of Bone and Mineral Metabolism. 2008;pp 208–13.
14. Tritos NA, Klibanski A. Effects of growth hormome on bone. Prog Mol Biol Transl Sci 2016;138:193–211.

15. Giustina A, Mazziotti G, Ganalis E. Growth hormone, insulin-like growth factors, and the skeleton. Endocr Rev 2008;29:535–59.



16. Bassett JH. Williams GR. Role of thyroid hormones in skeletal development and bone maintenance. Endocr Rev 2016;37:135–87.


17. Sundaraghavan V, Mazur MM, Evans B, Liu J, Ebraheim NA. Diabetes and bone health: latest evidence and clinical implications. Ther Adv Musculoskelet Dis 2017;9:67–74.



18. Castrogiovanni P, Trovato FM, Szychlinska MA, Nsir H, Imbesi R, Musumeci G. The importance of physical activity in osteoporosis. From the molecular pathways to the clinical evidence. Histol Histopathol 2016;31:1183–94.

19. Grover M, Bachrach LK. Osteoporosis in children with chronic illness. Diagnosis, monitoring, and treatment. Curr Osteoporos Rep 2017;15:271–82.


21. Henderson RC, Berglund LM, May R, Zemel BS, Grossberg RI, Johnson J, et al. The relationship between fractures and DXA measures of BMD in the distal femur of children and adolescents with cerebral palsy or muscular dystrophy. J Bone Miner Res 2010;25:520–6.


22. Fehlings D, Switzer L, Agarwal P, Wong C, Sochett E, Stevenson R, et al. Informing evidence-based clinical practice guidelines for children with cerebral palsy at risk of osteoporosis: a systematic review. Dev Med Child Neurol 2012;54:106–16.


23. Hough JP, Boyd RN, Keating JL. Systematic review of interventions for low bone mineral density in children with cerebral palsy. Pediatrics 2010;125:e670–8.


24. Iwasaki T, Nonoda Y, Ishii M. Long-term outcomes of children and adolescents who had cerebral palsy with secondary osteoporosis. Curr Med Res Opin 2012;28:737–47.


25. Rodd C, Lang B, Ramsay T, Alos N, Huber AM, Cabral DA, et al. Incident vertebral fractures among children with rheumatic disorders 12 months after glucocorticoid initiation: a national observational study. Arthritis Care Res (Hoboken) 2012;64:122–31.



27. Schmidt S, Mellstrom D, Norjavaara E, Sundh SV, Saalman R. Low bone mineral density in children and adolescents with inflammatory bowel disease: a population-based study from Western Sweden. Inflamm Bowel Dis 2009;15:1844–50.

28. El-Matary W, Sikora S, Spady D. Bone mineral density, vitamin D, and disease activity in children newly diagnosed with inflammatory bowel disease. Dig Dis Sci 2011;56:825–9.


29. Pappa H, Thayu M, Sylvester F, Leonard M, Zemel B, Gordon C. Skeletal health of children and adolescents with inflammatory bowel disease. J Pediatr Gastroenterol Nutr 2011;53:11–25.



30. Hogler W, Wehl G, van Staa T, Meister B, Klein-Franke A, Kropshofer G. Incidence of skeletal complications during treatment of childhood acute lymphoblastic leukemia: comparison of fracture risk with the General Practice Research Database. Pediatr Blood Cancer 2007;48:21–7.


31. Alos N, Grant RM, Ramsay T, Halton J, Cummings EA, Miettunen PM, et al. High incidence of vertebral fractures in children with acute lymphoblastic leukemia 12 months after the initiation of therapy. J Clin Oncol 2012;30:2760–7.


32. Lalayiannis AD, Crabtree NJ, Fewtrell M, Biassoni L, Milford DV, Ferro CJ, et al. Assessing bone mineralisation in children with chronic kidney disease: what clinical and research tools are available? Pediatr Nephrol 2020;35:937–57.


33. Helenius I, Remes V, Salminen S, Valta H, Makitie O, Holmberg C, et al. Incidence and predictors of fractures in children after solid organ transplantation: a 5-year prospective, population-based study. J Bone Miner Res 2006;21:380–7.


34. Johnston CC Jr, Miller JZ, Slemenda CW, Reister TK, Hui S, Christian JC, et al. Calcium supplementation and increases in bone mineral density in children. N Engl J Med 1992;327:82–7.


35. Lloyd T, Andon MB, Rollings N, Martel JK, Landis JR, Demers LM, et al. Calcium supplementation and bone mineral density in adolescent girls. JAMA 1993;270:841–4.


36. Winzenberg TM, Powell S, Shaw KA, Jones G. Vitamin D supplementation for improving bone mineral density in children. Cochrane Database Syst Rev 2010;(10):CD006944.


37. Greene DA, Naughton GA. Calcium and vitamin-D supplementation on bone structural properties in peripubertal female identical twins: a randomised controlled trial. Osteoporos Int 2011;22:489–98.


38. The Korean Nutrition Society. 2020 Dietary reference intakes for Koreans: application [Internet]. Seoul (Korea), The Korean Nutrition Society. [cited 2022 Feb 1]. Available from: http://www.kns.or.kr.
39. Rosen CJ, Abrams SA, Aloia JF, Brannon PM, Clinton SK, Durazo-Arvizu RA, et al. IOM committee members respond to Endocrine Society vitamin D guideline. J Clin Endocrinol Metab 2012;97:1146–52.



40. Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2011;96:1911–30.

41. Committee on Nutrition and the Council on Sports Medicine and Fitness. Sports drinks and energy drinks for children and adolescents: are they appropriate? Pediatrics 2011;127:1182–9.



42. Hind K, Burrows M. Weight-bearing exercise and bone mineral accrual in children and adolescents: a review of controlled trials. Bone 2007;40:14–27.


43. McKay HA, Petit MA, Schutz RW, Prior JC, Barr SI, Khan KM. Augmented trochanteric bone mineral density after modified physical education classes: a randomized school-based exercise intervention study in prepubescent and early pubescent children. J Pediatr 2000;136:156–62.


44. MacKelvie KJ, Khan KM, Petit MA, Janssen PA, McKay HA. A school-based exercise intervention elicits substantial bone health benefits: a 2-year randomized controlled trial in girls. Pediatrics 2003;112:e447.


45. Petit MA, McKay HA, MacKelvie KJ, Heinonen A, Khan KM, Beck TJ. A randomized school-based jumping intervention confers site and maturity-specific benefits on bone structural properties in girls: a hip structural analysis study. J Bone Miner Res 2002;17:363–72.


46. Specker B, Thiex NW, Sudhagoni RG. Does exercise influence pediatric bone? A systematic review. Clin Orthop Relat Res 2015;473:3658–72.



47. Field AE, Gordon CM, Pierce LM, Ramappa A, Kocher MS. Prospective study of physical activity and risk of developing a stress fracture among preadolescent and adolescent girls. Arch Pediatr Adolesc Med 2011;165:723–8.



48. Hohman EE, Balantekin KN, Birch LL, Savage JS. Dieting is associated with reduced bone mineral accrual in a longitudinal cohort of girls. BMC Public Health 2018;18:1285.



49. Baroncelli GI, Bertelloni S. The use of bisphosphonates in pediatrics. Horm Res Paediatr 2014;82:290–302.


50. Dwan K, Phillipi CA, Steiner RD, Basel D. Bisphosphonate therapy for osteogenesis imperfecta. Cochrane Database Syst Rev 2016;10:CD005088.


51. Alcausin MB, Briody J, Pacey V, Ault J, McQuade M, Bridge C, et al. Intravenous pamidronate treatment in children with moderate-to-severe osteogenesis imperfecta started under three years of age. Horm Res Paediatr 2013;79:333–40.


52. Baroncelli GI, Vierucci F, Bertelloni S, Erba P, Zampollo E, Giuca MR. Pamidronate treatment stimulates the onset of recover y phase reducing fracture rate and skeletal deformities in patients with idiopathic juvenile osteoporosis: comparison with untreated patients. J Bone Miner Metab 2013;31:533–43.


53. Bachrach LK, Ward LM. Clinical review 1: bisphosphonate use in childhood osteoporosis. J Clin Endocrinol Metab 2009;94:400–9.

54. Simm PJ, Biggin A, Zacharin MR, Rodda CP, Tham E, Siafarikas A, et al. Consensus guidelines on the use of bisphosphonate therapy in children and adolescents. J Paediatr Child Health 2018;54:223–33.


55. Ozel S, Switzer L, Macintosh A, Fehlings D. Informing evidence-based clinical practice guidelines for children with cerebral palsy at risk of osteoporosis: an update. Dev Med Child Neurol 2016;58:918–23.


56. Iwasaki T, Takei K, Nakamura S, Hosoda N, Yokota Y, Ishii M. Secondary osteoporosis in long-term bedridden patients with cerebral palsy. Pediatr Int 2008;50:269–75.


57. Thornton J, Ashcroft DM, Mughal MZ, Elliott RA, O'Neill TW, Symmons D. Systematic review of effectiveness of bisphosphonates in treatment of low bone mineral density and fragility fractures in juvenile idiopathic arthritis. Arch Dis Child 2006;91:753–61.



58. Acott PD, Wong JA, Lang BA, Crocker JF. Pamidronate treatment of pediatric fracture patients on chronic steroid therapy. Pediatr Nephrol 2005;20:368–73.


59. El-Husseini AA, El-Agroudy AE, El-Sayed MF, Sobh MA, Ghoneim MA. Treatment of osteopenia and osteoporosis in renal transplant children and adolescents. Pediatr Transplant 2004;8:357–61.


60. Sbrocchi AM, Forget S, Laforte D, Azouz EM, Rodd C. Zoledronic acid for the treatment of osteopenia in pediatric Crohn's disease. Pediatr Int 2010;52:754–61.


61. Gordon KE, Dooley JM, Sheppard KM, MacSween J, Esser MJ. Impact of bisphosphonates on survival for patients with Duchenne muscular dystrophy. Pediatrics 2011;127:e353–8.


62. Sbrocchi AM, Rauch F, Jacob P, McCormick A, McMillan HJ, Matzinger MA, et al. The u s e of i nt r ave nou s bisphosphonate therapy to treat vertebral fractures due to osteoporosis among boys with Duchenne muscular dystrophy. Osteoporos Int 2012;23:2703–11.


63. Lee JM, Kim JE, Bae SH, Hah JO. Efficacy of pamidronate in children with low bone mineral density during and after chemotherapy for acute lymphoblastic leukemia and non-Hodgkin lymphoma. Blood Res 2013;48:99–106.



64. Carpenter PA, Hoffmeister P, Chesnut CH 3rd, Storer B, Charuhas PM, Woolfrey AE, et al. Bisphosphonate therapy for reduced bone mineral density in children with chronic graft-versus-host disease. Biol Blood Marrow Transplant 2007;13:683–90.


65. Suresh E, Pazianas M, Abrahamsen B. Safety issues with bisphosphonate therapy for osteoporosis. Rheumatology (Oxford) 2014;53:19–31.









