Comparison between transient and permanent congenital hypothyroidism on a thyroid function test after re-evaluation
Article information
Abstract
Purpose
Congenital hypothyroidism (CH) is diagnosed with neonatal screening and is treated early in the neonatal period. Among these patients, transient CH (TCH) is included and requires re-evaluation. The purpose of this study was to find the best way to discontinue levothyroxine and to find trends in thyroid function tests (TFTs) after re-evaluation.
Methods
We retrospectively reviewed 388 patients diagnosed with CH. They were classified as permanent CH (PCH) and TCH. The total number of the PCH and TCH groups was 83 (51 boys and 32 girls). We compared clinical parameters to predict TCH and to identify the trends of TFT.
Results
The first thyroid-stimulating hormone (TSH) value after discontinuation and the average TSH value for 1, 2, and 3 years were all significantly higher in the PCH group (P<0.01). The first fT4 value after discontinuation and the average fT4 value for 1, 2, and 3 years were all significantly higher in the TCH group (P<0.01). The optimal cutoff value on the receiver operating characteristic curve for PCH prediction with an average of 3 years of TSH was greater than 9.05 μIU/mL, which was predicted with a sensitivity of 100% and a specificity of 100%.
Conclusions
When the TSH value ranges from 10 μIU/mL to 20 μIU/mL, clinicians can discontinue levothyroxine if the next result is around 10 μIU/mL or shows a decreasing trend.
Highlights
· Our study aimed to find trends in thyroid function test after re-evaluation and to find out the best way to discontinue levothyroxine. Our findings show that even if the thyroid-stimulating hormone value ranges from 10 μIU/mL to 20 μIU/mL, clinicians can keep discontinuing levothyroxine.
Introduction
Congenital hypothyroidism (CH) is a common pediatric endocrine disease included in neonatal screening tests and requires lifelong medication. Regardless of the etiology, if treatment is successful, there are no sequelae such as intellectual disability [1]. As newborn screening tests are becoming more common in many countries, the number of diagnosed CH cases is increasing [2-4]. These patients can be subclassified as transient CH (TCH) or permanent CH (PCH). Identification of TCH can provide patients with economic and time benefits. To differentiate these disease types, the current guidelines recommend re-evaluation of thyroid function at the age of 2 to 3 years [5,6].
The current guidelines recommend that cases with thyroidstimulating hormone (TSH) level exceeding 10 μIU/mL after 4 weeks of treatment discontinuation be considered PCH. In addition, if the TSH value is outside the normal range but less than 10 μIU/mL and the free thyroxine (fT4) is in the normal range, a retest is suggested after 3 to 4 weeks [5].
The definition of TCH is not clear according to the current guidelines. Kang et al. [7] defined TCH as thyroid function test (TFT) result in the acceptable range (TSH <10 μIU/ mL and normal fT4 level) for at least 6 months. Razavi and Mohammadi [8] defined the condition as TCH if the TFT result was in the acceptable range (TSH <10 μIU/mL and normal free T4 level) for at least 12 weeks. Other studies defined TCH as a normal initial TFT result [9-14].
However, according to our study, a high initial TSH level can gradually stabilize, allowing levothyroxine to be discontinued. Accordingly, some patients could be diagnosed with TCH even if the TSH level is greater than 10 μIU/mL. On the other hand, even if the initial TSH level was normal, if it increased sharply or the fT4 level decreased, levothyroxine should be readministered. Therefore, it was difficult to determine PCH with only one test result of a TSH level over 10 μIU/mL. Moreover, there were subjects whose TFT results were in the acceptable ranges (TSH <10 μIU/mL and normal fT4 level) for 6 months but then increased to greater than 20 μIU/mL.
Our study aimed to find trends in TFT after re-evaluation and to define TCH in a more definitive way than previous studies.
Materials and methods
1. Subjects
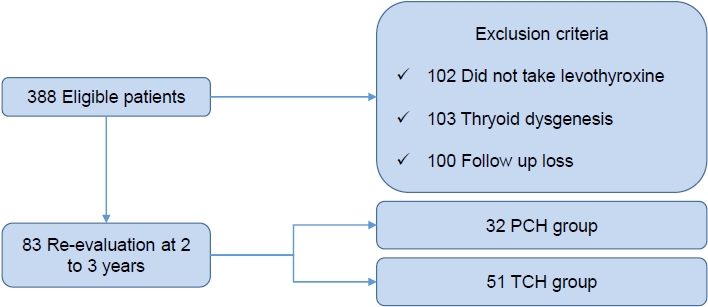
This research was conducted at Chonnam National University Hospital (CNUH). The charts of patients who had visited CNUH with CH from January 2004 to December 2020 were retrospectively reviewed. The study was approved by the Institutional Review Board of Chonnam National University Hospital (approval number: CNUH-2022-051). During this period, 388 subjects were diagnosed with CH. Among these patients, we excluded 102 patients who did not take levothyroxine, 103 with thyroid dysgenesis including agenesis, and 100 who were lost to follow up.
PCH and TCH were classified as follows. PCH was defined as: (1) TSH level 20 μIU/mL or higher; (2) TSH level over 10 μIU/mL with fT4 level below the normal range; and (3) clinical symptoms of hypothyroidism requiring levothyroxine. TCH was defined as TSH and fT4 levels in the normal range on 2 or more consecutive tests in 1 year (Fig. 1).
2. Method
During treatment with levothyroxine for all patients, periodic follow-up and drug dose adjustment were performed according to current guidelines [5,6]. Treatment was administered until the age of 2 to 3 years. Re-evaluation of TSH and fT4 levels was performed after discontinuing levothyroxine. If the test result was normal, the patients was maintained on follow-up; if the result was abnormal, the treatment was readministered. Even if the TSH level was over 10 μIU/mL, we did not restart treatment if the fT4 level was normal and there were no clinical symptoms. PCH and TCH were classified based on the criteria described above. Gestational age, fT4, TSH at the time of diagnosis, birth weight, and diet were analyzed. To identify trends of TSH and fT4 levels after discontinuing levothyroxine, ROC analysis was performed for initial, 1-year, 2-year, and 3-year average levels of TSH and fT4. The time period required to determine PCH and TCH also was measured.
3. Laboratory measurement
Serum fT4 and TSH concentrations were measured using radioimmunoassays. The range of normal values was defined based on 2 standard deviations of the test results performed in the participating hospital. The ranges were 0.64–6.27 μIU/mL for TSH and 0.89–1.76 ng/dL for fT4.
4. Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). P-values under 0.05 were considered statistically significant. To compare clinical parameters of PCH and TCH groups, Student t-test was performed for sex, screening test, gestational age, and birth weight. To evaluate the optimal cutoff values of TSH and fT4, we performed receiver operating characteristic (ROC) analyses. The optimal values were measured by calculating the Youden index (J), which is the maximum vertical distance between the ROC curve and the reference line [maximum (sensitivity + specificity -1)] [15].
Results
1. Comparison of clinical parameters and levothyroxine doses of PCH and TCH groups
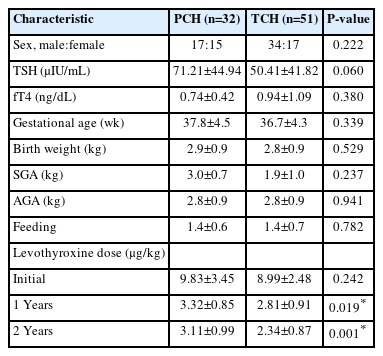
Our study enrolled 83 subjects (51 boys and 32 girls) and divided them into 2 groups. Thirty-two subjects (39%) were classified as the PCH group and 51 subjects (61%) were classified as the TCH group. No clinical parameters were significantly different between the groups (Table 1). There was no significant difference in sex between PCH and TCH groups (P=0.222). The average TSH level at the time of diagnosis was higher in the PCH group, but there was no significant difference (P=0.06). The average fT4 level at the time of diagnosis was higher in the TCH group, but there was no significant difference (P=0.38). In feeding, we set 0 points for formula, one point for mixed feeding, and 2 points for breastfeeding only. The average value was 1.42 in the PCH group and1.37 in the TCH group, which was not a significant difference (P=0.782). The average gestational age and birth weight were not significantly different between the 2 groups. There were 2 small for gestational age 2 subjects (8%) in the PCH group and 4 (9%) in the TCH group, with no significant difference (P=0.237). There were 22 appropriate for gestational age subjects (92%) in the PCH group and 39 (89%) in the TCH group, with no significant difference (P=0.941). There were no large for gestational age (LGA) subjects in the PCH group and one LGA subject (2%) in the TCH group. The initial levothyroxine dose was not significantly different between the 2 groups (P=0.242), though the levothyroxine dose at the first and second years was significantly lower in the TCH group (Table 1).
2. Comparison of initial and average values of TSH and fT4
Initial and average values of TSH and fT4 after discontinuation were significantly different (P<0.01) (Table 2). The optimal cutoff value of initial TSH level on the ROC curve for PCH prediction was 7.79 μIU/mL, which could be predicted with a sensitivity of 87.5% and a specificity of 86.3%. The optimal cutoff value of initial fT4 level for TCH prediction was 1.07 ng/dL, which could be predicted with a sensitivity of 86.3% and a specificity of 68.7%.
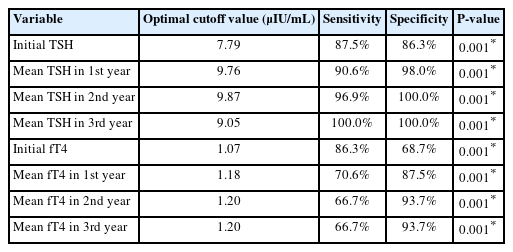
Comparison of initial and average values of TSH and fT4 between PCH and TCH, using receiver operating characteristic analyses
The optimal cutoff value on the ROC cur ve for PCH prediction based on average 1-year TSH was 9.76 μIU/mL, which could be predicted with a sensitivity of 90.6% and a specificity of 98%. The optimal cutoff value based on average 2-year TSH was 9.87 μIU/mL, which could be predicted with a sensitivity of 96.9% and a specificity of 100%. The optimal cutoff value using average 3-year TSH was 9.05 μIU/mL, with a sensitivity of 100% and a specificity of 100% (Fig. 2). The optimal cutoff value for TCH prediction with average 1-year fT4 was 1.18 ng/dL, with a sensitivity of 70.6% and a specificity of 87.5%. The optimal cutoff value with 2-year fT4 average was 1.20 ng/dL, with a sensitivity of 66.7% and a specificity of 93.7%. The optimal cutoff value using average 3-year fT4 was 1.20 ng/dL, which could be predicted with a sensitivity of 66.7% and a specificity of 93.7% (Fig. 3).
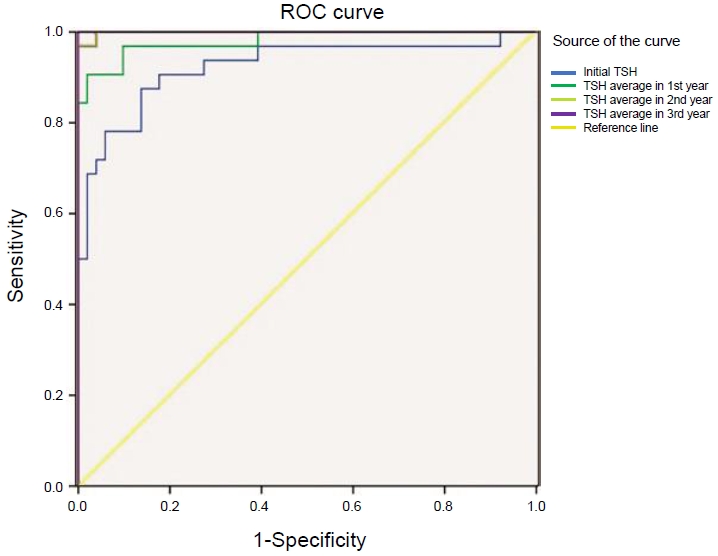
Receiver operating characteristic (ROC) curves of initial (area under the curve [AUC], 0.923; 95% confidence interval [CI], 0.857–0.990), 1-year (AUC, 0.980; 95% CI, 0.000–1.000), 2-year (AUC, 0.999; 95% CI, 0.000–1.000), and 3-year (AUC, 1.000; 95% CI, 1.000–1.000) averages of thyroid stimulating hormone (TSH) for predicting permanent congenital hypothyroidism.
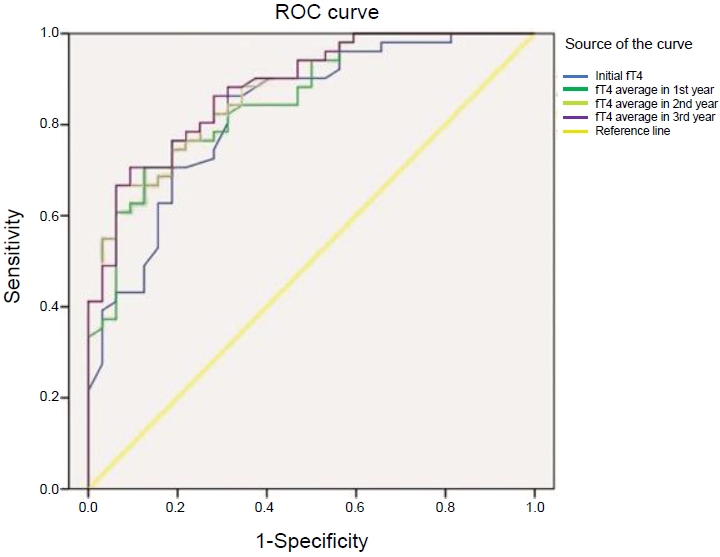
Receiver operating characteristic (ROC) curves of initial (area under the curve [AUC], 0.828; 95% confidence interval [CI], 0.738–0.918), 1-year (AUC, 0.856; 95% CI, 0.776–0.936), 2-year (AUC, 0.876; 95% CI, 0.804–0.948), and 3-year (AUC, 0.881; 95% CI, 0.811–0.952) averages of free thyroxine (fT4) for predicting transient congenital hypothyroidism.
During the follow-up period, 37 subjects had a TSH level greater than 10 μIU/mL. Five subjects had normal TFT results for longer than 1 year and were classified as TCH.
3. Durations required to classify PCH and TCH
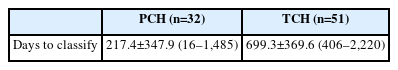
The average period required for classification was 217.4 days for PCH and 699.3 days for TCH (Table 3). However, an average of 1,392 days was needed to classify 79 of the 83 subjects (95%) as PCH and TCH.
Discussion
CH can be classified as athyreosis, dysgenesis, and dyshormonogenesis, among which dyshormonogenesis has the smallest therapeutic dose [16]. Dyshormonogenesis can be subcategorized as PCH and TCH. And there is no apparent difference between them. Accordingly, it is not easy to distinguish. Although various molecular genetic studies are being conducted, the cost is high and few conclusive data have been collected [17-19].
The levothyroxine dose during treatment is the most studied factor to differentiate between PCH and TCH. Many studies show that the lower is the treatment dose, the higher is the possibility of TCH [8-14,20-25]. The same result was found in our study. Another study found that TSH or fT4 level at screening and family history can predict TCH [11-13,21,23,25]. Studies have shown that low levothyroxine doses during treatment can lead to discontinuation due to resolution before 3 years of age [10,14,20,25]. However, due to the risk of neurodevelopmental problems, it is recommended to not discontinue treatment until after 3 years of age [5,8].
Distinction between PCH and TCH often is based on a single TFT after treatment discontinuation [9,11-13,24]. Though there is no confirmative standard for differentiating between PCH and TCH, the current guideline suggests PCH if the TSH value exceeds 10 μIU/mL after stopping treatment [5]. In other studies about PCH and TCH, TSH level cutoffs were set at 10 μIU/mL, 15 μIU/mL, or 7 μIU/mL for PCH [20-23,25].
In our study, even if the TSH level was 10 μIU/mL or higher, we discontinued levothyroxine considering the subject's clinical symptoms and fT4 level. After discontinuation, 5 subjects maintained normal levels of TSH and fT4 for more than 1 year, which we categorized as TCH. Furthermore, if normal levels of TSH and fT4 persisted for 1 year, TSH elevation or symptoms of hypothyroidism did not recur. However, in one subject with distal monosomy 10q, the TSH and fT4 levels were normal for 1 year, increased to greater than 10 μIU/mL for 1 year, and then stabilized to normal levels.
The longest period of consecutive normal values in the PCH group was 281 days, longer than 6 months. Therefore, criteria were established for TCH when 2 or more consecutive normal values of TSH and fT4 were maintained for 1 year.
In some subjects, re-evaluation was continued even when the TSH level was greater than 20 μIU/mL. In most cases, the TSH level increased or persisted, requiring restart of levothyroxine. However, in one case, the TSH level was higher than 20 μIU/mL due to a cold, after which the subject maintained normal TSH and fT4 levels for 1 year and was confirmed to have TCH. Wong et al. [26] insisted that TSH elevation is regularly associated with hypothyroidism but can be a result of acute disease. Therefore, we did not restart treatment considering the patient's acute disease despite a TSH level higher than 20 μIU/mL.
Statistical analysis of our study revealed distinction of PCH and TCH in the initial test in most cases. Irrespective of the initial test result, TSH changed from abnormal to normal in some cases or from normal to abnormal levels in others. Based on annual average results, the TCH group showed a stabilizing pattern over the study period. However, in the PCH group, inconsistent TSH values were repeated and thereafter, gradually increased.
Annual average values of both TSH and fT4 showed significant difference between the PCH group and the TCH group. The optimal cutoff value of TSH clearly showed higher sensitivity and specificity than that of fT4. In most of cases, fT4 level below the normal range was accompanied by an increase in TSH level.
In our study, goiter occurred after discontinuation of levothyroxine, resulting in readministration [5]. Another study confirmed normal levels of TSH and fT4 immediately after drug discontinuation [27]. However, with time, goiter appeared and an elevated TSH level was reported. In other studies, goiter and nodules occurred among patients with dyshormonogenesis, some of which progressed to malignacy [28,29]. In our study, 1 patient developed papillary thyroid cancer while receiving treatment for CH and eventually had to undergo total thyroidectomy. According to that finding, if there is goitrous CH due to dyshormonogenesis, the TSH level should be reduced to the normal range and periodic ultrasound of the neck is required [30].
This study had limitations due to its retrospective nature and small number of subjects. In addition, if it had defined PCH or TCH differently, the results may have been different. Therefore, more research is needed on definitions of PCH and TCH. With a larger number of subjects, more valuable research results could be obtained.
According to our study, it is difficult to determine PCH and TCH with one test after re-evaluation. Even if normal values are presented in the initial test, later test results can be abnormal. Accordingly, a certain period of time is required for confirming PCH and TCH. The TSH and fT4 level can be inconsistent or stabilized to normal level, and that would be the point which we can distinguish between PCH and TCH. Our findings show that, even if TSH exceeds 10 μIU/mL, levothyroxine does not have to be restarted, and additional tests should be performed. A subsequent TSH level less than 20 μIU/mL and repeated measures of approximately 10 μIU/mL support the choice to not restart treatment. The patient's condition and clinical symptoms should also be considered. Based on our findings, the average TSH level is a good parameter for predicting TCH.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data availability
The data that support the findings of this study can be provided by the corresponding author upon reasonable request.
Author contribution
Conceptualization: SHL, HGL, EMY, CJK; Data curation: SHL, HGL, EMY, CJK; Formal analysis: SHL, HGL, CJK; Funding acquisition: SHL, CJK; Methodology: SHL, HGL, EMY, CJK; Project administration: SHL, HGL, EMY, CJK; Visualization: SHL, EMY, CJK; Writing - original draft: SHL; Writing - review & editing: SHL, HGL, EMY, CJK