Association Kikuchi disease with Hashimoto thyroiditis: a case report and literature review
Article information
Abstract
Kikuchi-Fujimoto disease (KFD) is a benign and self-limited disease characterized by fever and lymphadenopathy. The etiology of KFD is unknown, but an autoimmune cause has been suggested. Hashimoto thyroiditis is the most common autoimmune thyroid disorder in children and is known to be associated with other autoimmune diseases. Only a few cases of Hashimoto thyroiditis associated with KFD have been documented. We report a case of a 16-year-old girl who was first diagnosed with KFD and developed Hashimoto thyroiditis 2 years and 6 months later during her follow-up period. Physicians of patients with KFD should consider the possibility of autoimmune diseases like Hashimoto’s thyroiditis.
Introduction
Kikuchi-Fujimoto disease (KFD), or histiocytic necrotizing lymphadenitis, is a benign, self-limiting disease characterized by fever and regional lymphadenopathy, especially in the cervical region [1]. KFD is a rare disease in both adults and children, commonly seen in young Asian women [2]. Although many studies on KFD have been reported, the etiology and pathogenesis of KFD remain unclear. Clinical and histologic features of KFD are similar to those of systemic lupus erythematosus (SLE), and some authors suggest that KFD could have an autoimmune origin [3].
Hashimoto thyroiditis is currently the most common autoimmune thyroid disorder in children and adolescents. Circulating antibodies against thyroid peroxidase (anti-TPO Ab) and antithyroglobulin antibody (anti-Tg Ab) are found in patients with Hashimoto thyroiditis [4]. Clinical manifestations at the time of presentation vary depending on the nature of the antithyroid antibodies, and may include asymptomatic goiter, symptoms of hypothyroidism, or transient hyperthyroidism [5]. Previously published studies have reported an association between KFD and other autoimmune disorders, including thyroiditis, SLE, and Sjogren's syndrome [6]. Recently, Kang et al. [7] reported that of 86 children and adolescents who were diagnosed with KFD, 2 were also found to be afflicted with thyroiditis. However, there have been few reports about the potential relationship between Hashimoto thyroiditis with KFD [8,9]. Therefore, we report a case of Hashimoto thyroiditis in a girl with a history of KFD.
Case report
An 11-year-old girl with no significant past medical history was referred to our institution for evaluation of lymphadenopathy on both sides of her neck that was noticed about 3 weeks before the examination, and the patient complained of mild pain and tenderness locally. She also reported a history of persistent fever of 1 week’s duration before admission. The patient was febrile without any clinical evidence of systemic or oropharyngeal infection, but there were multiple lymph nodes enlargements on both sides of her neck, most of which were levels II and IV on the right side. Thyroid gland was not enlarged on physical examination. There was no family history of lymphoma, leukemia, SLE, rheumatoid arthritis, or any other autoimmune disorder. Her white blood cell count was 2.12×109/L, and it consisted of 52.2% neutrophils, 37.3% lymphocytes, and 3.8% monocytes. Her hemoglobin level was 12.1 g/dL and platelet level was 211×109/L. Her serum erythrocyte sedimentation rate was 35 mm/hr, C-reactive protein was 1.06 mg/dL, electrolyte level and liver function tests were normal. Herpes simplex virus, Epstein Barr virus, Toxoplasma, and cytomegalovirus serologies were negative. Rheumatoid factor, complement 3 (C3), complement 4 (C4), antinuclear antibody (ANA), and antidouble stranded DNA levels were within normal limits. A computed tomography of the neck revealed right side dominant multiple heterogeneous enhancing conglomerated enlarged lymph nodes in both neck at levels II, III, IV, and V (Fig. 1). Bone marrow aspiration was negative for malignancy and bacterial culture studies were also negative. The thyroid function test was not performed because she did not show any evidence of goiter. Intravenous 3rd generation cephalosporin was initially administered, but spiking fever persisted. Three days after admission, an excisional biopsy of the enlarged cervical lymph node was performed. The biopsy demonstrated irregular paracortical areas of coagulative necrosis with abundant karyorrhectic debris, which were compatible with KFD. Based on the diagnosis of KFD and persistence of fever, oral prednisolone (1 mg/kg/day) treatment was started. Two days later, the fever disappeared and the size of lymph nodes began to decrease gradually.

Axial contrast-enhanced computed tomography of the neck show multiple heterogeneous enlarged lymph nodes in both neck. The maximum size of the lymph nodes in both neck at levels II (A; arrow) and IV (B).
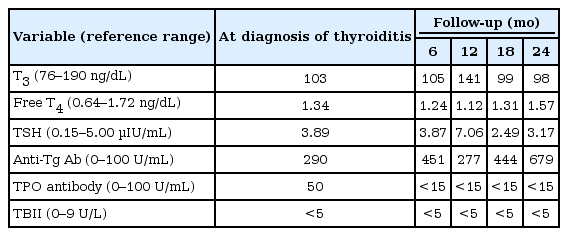
The patient did not experience any additional recurrence of KFD. Two years and 6 months later, she presented with evidence of goiter. She had first noticed the enlarged thyroid gland 3 weeks ago. Goiter size was measured in grade Ia by World Health Organization criteria [10]. The thyroid gland was palpable and it was diffusely enlarged but not visible. Although thyroid function tests were within normal limits, antithyroglobulin antibody (anti-Tg) were positive: anti-Tg Ab, 290 U/mL (normal, <100 U/mL); thyroid peroxidase antibody (anti-TPO), 50 U/mL (normal, <100 U/mL); TSH-binding immunoglobulin, <5 U/L (normal, <9 U/L). Rheumatoid factor and ANA titer were negative. She was diagnosed with Hashimoto’s thyroiditis several years after diagnosed with KFD. She is now 16 years old and is doing well. She undergoes regular check-up every 6 months and is not taking any medication (Table 1).
This study was waived by the Institutional Review Board of Ajou University School of Medicine (AJIRB-MEDEXP-18-052).
Discussion
KFD is a rare, self-limiting, benign, systemic lymphadenitis, which has a higher prevalence in Asian women. The most common clinical findings consist of persistent fever and localized lymphadenopathy [11]. KFD usually resolves spontaneously over a period of several weeks to months. However, a few patients with KFD showed poor clinical outcomes, thought to be attributable to systemic involvement [12,13]. The exact etiology of KFD is still unknown. Initially, a viral infection was suspected to be the etiology of KFD due to flu-like symptoms. Several viruses were thought to be implicated in the pathogenesis of KFD, but their presence was not demonstrated and their involvement remains controversial [14]. No viral and bacterial infection was also found in our case. On the other hand, based on the clinical (fever, lymphadenitis, skin rash, and arthralgia) and histologic similarity (paracortical necrosis with karyorrhectic debris and inflammatory cell responses) between KFD and SLE, an autoimmune etiology was proposed [6]. In addition, several cases of KFD associated with other autoimmune diseases have been reported, these reports support the hypothesis that KFD has an autoimmune origin [3,15]. Kim et al. [16] reported that the development of autoimmune disease was diagnosed in approximately 4% in children with KFD. In an adult study, 7% of KFD patients had autoimmune disease [17]. Although the exact mechanism by which KFD and other autoimmune disease were related is unknown, but based on laboratory and histological findings, it has been hypothesized that KFD might represent an exuberant T-cell-mediated response to certain antigen stimuli in genetically susceptible individuals [14].
Hashimoto thyroiditis with goiter is one of the most common causes of thyroid disease in children and adolescents. It is associated with circulating antibodies against anti-TPO Ab and anti-Tg Ab and is characterized by lymphocytic infiltration of the thyroid gland, which results in asymmetric thyroid enlargement [4]. Clinical manifestations at the time of presentation vary depending on the nature of the antithyroid antibodies, including asymptomatic goiter, symptoms of hypothyroidism, or transient hyperthyroidism [5]. Hashimoto thyroiditis is an organ-specific autoimmune disease and the antithyroid immune response begins with activation of thyroid antigen-specific helper T cells. In previous studies of children, Hashimoto thyroiditis is found to be linked to organ-specific autoimmune diseases (such as vitiligo, myasthenia gravis, and thrombocytopenic purpura), systemic autoimmune diseases (such as rheumatoid arthritis, SLE, and progressive systemic sclerosis), and other autoimmune endocrine diseases (such as insulin-dependent diabetes mellitus and autoimmune hypoparathyroidism) [18].
A few cases of KFD associated with Hashimoto thyroiditis have been reported [8,15]. In a majority of the cases previously reported, KFD and Hashimoto thyroiditis occurred concurrently. In 3 cases, however, KFD occurred later in patients who were previously diagnosed with Hashimoto thyroiditis [3,9,19]. The reported cases are presented in Table 2. Our patient had a previous history of KFD and was diagnosed with Hashimoto thyroiditis 2 years and 6 months later, which is different from other cases. In some cases, autoimmune disorders such as SLE developed from few months to 5 years after diagnosed with KFD [2,3]. From this point of view, KFD may be associated with the development of Hashimoto's thyroiditis and other autoimmune disorders. Our case report had limitations. We did not examine thyroid hormones and antibodies at the time of diagnosis of KFD because the patient had no evidence of goiter; we did not, at the time, consider a possible of the association between autoimmune thyroiditis and KFD. So, we did not know the exact timing of autoimmune thyroiditis. Based on our case, we suggest that patients with KFD may need to check the thyroid function tests at the time of initial diagnosis.
In conclusion, health care providers treating patients diagnosed with KFD should consider the possibility of autoimmune diseases or concurrent autoimmune disease, even though cases of Hashimoto thyroiditis with associated KFD has been relative rare. Therefore, it may be necessary to monitor the thyroid function of patients diagnosed with KFD for the possible later development of autoimmune disease such as Hashimoto thyroiditis.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.