 |
 |
- Search
| Ann Pediatr Endocrinol Metab > Volume 28(Suppl 1); 2023 > Article |
|
· Our case highlights the importance of a thyroid diagnostic work-up. Clinicians must consider the possibility of DICER1 syndrome in a child or an adolescent who presents with thyroid diseases in addition to other common neoplasms.
To the editor,
DICER1 syndrome is a rare, autosomal-dominant, familial disorder that predisposes an individual to both benign and malignant tumors in multiple organs [1]. Carriers of the germline mutation in DICER1 are found at a prevalence of approximately 1/10,600 [2]. The clinical phenotypes of DICER1 mutations include pleuropulmonary blastoma, ovarian sex cordstromal tumors, cystic nephroma, thyroid gland neoplasia (multinodular goiter [MNG], adenomas or differentiated thyroid cancer), ciliary body medulloepithelioma, embryonal rhabdomyosarcoma, nasal chondromesenchymal hamartoma, pituitary blastoma, and pineoblastoma [1]. The DICER1 gene is located on chromosome 14q32.13 and is mainly involved in protein translation. Most of the DICER1 mutations cause the synthesis of abnormally short, inactive DICER protein. Accumulation of the inactive protein eventually leads to a loss of tumor suppression. Germline mutations in DICER1 have been identified in children and young adults with distinctive dysontogenetic hyperplastic or overtly malignant conditions [3].
We describe a case of an 8-year-old girl with DICER1 syndrome, which has rarely been reported in Korea. An 8-year-old girl visited us after magnetic resonance imaging of the abdomen revealed a heterogeneous mass in the left kidney. The patient was subsequently diagnosed with diffusely anaplastic Wilms tumor. At the age of 12, a palpable mass of the right thyroid lobe with thyroid nodules was detected. Intraoperatively, the patient was diagnosed with follicular thyroid adenoma (FTA). At the age of 13, the patient had a palpable mass of the left thyroid lobe, causing a progressively enlarged thyroid gland. A total thyroidectomy was performed. The patient was histopathologically diagnosed with adenomatous goiter with cystic change. She was concurrently found to have a follicular cyst in the left ovary, cystic lesion in the right middle lobe of the lung, and air-trappings in both lungs. These findings suggested an underlying DICER1 mutation.
On family history, the patient's maternal grandmother and aunt had a diagnosis of MNG. The patient underwent whole exome sequencing (WES) for a cancer predisposing syndrome, including DICER1 syndrome. The sequencing identified a heterozygous missense mutation, c.3506C>G (p.S1169*), in exon 21 of the DICER1 gene (Fig. 1A). Sanger sequencing was performed to confirm the DICER1 variant and to examine whether the patient's family members had a mutation in the same DICER1 exon. The patient's mother was also positive for the DICER1 pathogenic variant. Two siblings and the patient's father were negative for the genetic variant. The patient's maternal grandmother and aunt were suspected of having a mutation in the same DICER1 exon. However, they could not be evaluated further due to their personal situations. The patient's family tree is shown in Fig. 1B.
At the age of 14, the patient presented with severe enlargement of the right kidney and cysts with multiple septa. Biopsy after right total nephrectomy showed cystic nephroma. At the age of 16, the patient had developed nasal chondromesenchymal hamartoma.
The current case is characterized by thyroid manifestations of the DICER1 syndrome accompanied by common associated neoplasms. This patient's clinical experience is consistent with previous studies [3-5]. Thyroid manifestations of the DICER1 syndrome have been well described in the literature [6]. DICER1 is a key player in the normal development of the thyroid gland; multiple thyroid abnormalities have been identified in patients with DICER1 syndrome. Individuals who carry the DICER1 germline mutation are at increased risk of multinodular thyroid hyperplasia, which is the most highly penetrant phenotype of the thyroid disorder. This is especially notable in women with the mutation [7]. It was initially thought that the thyroid manifestations of DICER1 syndrome are restricted to MNG or FTA. However, an increasing number of population-based studies have revealed that a broad spectrum of thyroid diseases, ranging from benign conditions to the most aggressive thyroid cancers, can occur in DICER1 syndrome [8]. Lee et al. [9] suggested that diagnosis of DICER1 syndrome may be more common than previously thought if genetic testing was performed following histopathologic thyroid examinations in pediatric cases of thyroid diseases.
In conclusion, our case demonstrates the longitudinal time course of DICER1 syndrome, which has not been described in the Korean literature (Table 1). The study highlights the importance of a diagnostic thyroid work-up. Clinicians must consider the possibility of DICER1 syndrome in a child or an adolescent who presents with thyroid diseases in addition to other common neoplasms.
Notes
Fig. 1.
Results of whole exome sequencing (WES) and the patient's family tree. H, heterozygous missense mutation; N, normal; +, heterozygous missense mutation; -, no mutation; NA, no analysis. (A) Both the patient and her mother had a heterozygous missense mutation, c.3506C>G (p.S1169*), in exon 21 of the DICER1 gene (black color, square box, and arrow indicate multinodular goiter, DICER1 mutation [c.3506C>G, p.S1169*], and mutated nucleotides, respectively). (B) The arrow indicates the patient.
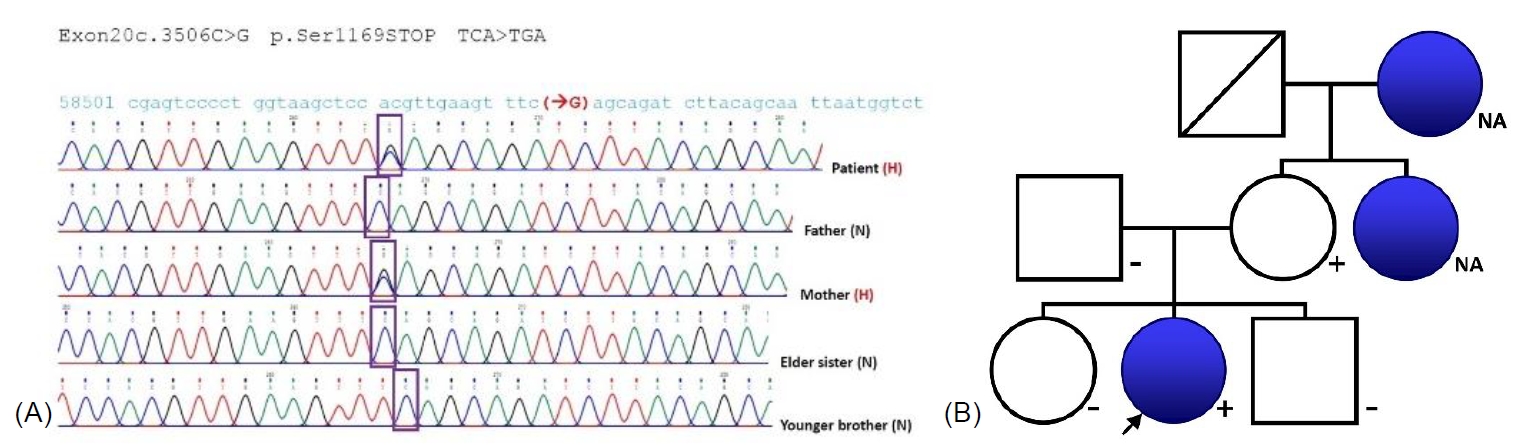
Table 1.
Longitudinal course of the current case
References
1. Schultz KAP, Williams GM, Kamihara J, Stewart DR, Harris AK, Bauer AJ, et al. DICER1 and associated conditions: identification of at-risk individuals and recommended surveillance strategies. Clin Cancer Res 2018;24:2251–61.




2. Kim J, Field A, Schultz KAP, Hill DA, Stewart DR. The prevalence of DICER1 pathogenic variation in population databases. Int J Cancer 2017;141:2030–6.




3. Choong CS, Priest JR, Foulkes WD. Exploring the endocrine manifestations of DICER1 mutations. Trends Mol Med 2012;18:503–5.


4. Stewart DR, Best AF, Williams GM, Harney LA, Carr AG, Harris AK, et al. Neoplasm risk among individuals with a pathogenic germline variant in DICER1. J Clin Oncol 2019;37:668–76.



5. Moke DJ, Thomas SM, Hiemenz MC, Nael A, Wang K, Shillingford N, et al. Three synchronous malignancies in a patient with DICER1 syndrome. Eur J Cancer 2018;93:140–3.



7. Oliver-Petit I, Bertozzi AI, Grunenwald S, Gambart M, Pigeon-Kerchiche P, Sadoul JL, et al. Multinodular goitre is a gateway for molecular testing of DICER1 syndrome. Clin Endocrinol 2019;91:669–75.


- TOOLS
- Related articles in APEM







