Pediatric and adult osteoporosis: a contrasting mirror
Article information
Abstract
Pediatric osteoporosis (PO) is a condition that is currently gaining recognition. Due to the lack of official definitions over the past few decades, the exact incidence of PO is unknown. The research does not provide a specific prevalence of PO in different world regions. However, this is expected to change with the latest 2019 guidelines proposed by the International Society of Clinical Densitometry. Although adult osteoporosis (AO) has been postulated a pediatric disease because its manifestation in adulthood is a result of the bone mass acquired during childhood, differences between PO and AO should be acknowledged. AO is defined as low bone density; however, PO is diagnosed based on existing evidence of bone fragility (vertebral fractures, pathological fractures). This is particularly relevant because unlike in adults, evidence is lacking regarding the association between low bone density and fracture risk in children. The enhanced capacity of pediatric bone for reshaping and remodeling after fracture is another difference between the two entities. This contrast has therapeutic implications because medication-free bone reconstitution is possible under certain conditions; thus, background therapy is not always recommended. In this narrative review, differences between PO and AO in definition, assessment, and medical approach were investigated.
Highlights
· Adult osteoporosis (AO) and pediatric osteoporosis (PO) differ in diagnosis – AO based on low bone density, PO on evidence of bone fragility. Unlike adults, the link between low bone density and fractures in children lacks evidence. This distinction extends to therapy, where medication-free bone reconstitution is an option in some cases, challenging conventional approaches.
Introduction
Pediatric osteoporosis (PO) has been recognized for many years with the first reports dating back to the 60’s [1]. However, the first proper and official definition of PO was published only in 2003 by the International Society of Clinical Densitometry (ISCD) task force [2]. Since then, the definition has been updated twice, once in 2013 and again in 2019 [3,4]. In contrast, eight Position Development Conferences on adult osteoporosis (AO) occurred between 2001 and 2019 [3,5-7].
Because PO occurs in dynamically growing bones, distinctions from AO have been identified. From the biomaterial or architectural aspect, bones in adults and children are distinct, making the latter a more complex entity [8].
Bone health in children is important and has implications; Chesnut [9] in 1989 stated that senile osteoporosis is a pediatric disease and rooted in childhood. Bone health in children was often forgotten, neglected, and undervalued during the last decades [10,11]. Compared with AO, PO remains unclear even among pediatricians because screening is often lacking and interpretation of the results can be incorrect [11].
Although bone densitometry assessment in adults is used to predict fracture risk and assess treatment response, its role and function in children remain ambiguous. The definition of osteoporosis in children is not based on bone mineral density (BMD) values as in adults. The ISCD has provided guidelines to rheumatologists and pediatricians, although some of the recommendations were based on expert opinion due to the scarcity of data on many topics.
Identifying children at risk of low bone density and bone fragility facilitates appropriate monitoring, management, and care.
In this review, the main differences between PO and AO in definition, assessment, monitoring, and treatment options are evaluated.
Definition of osteoporosis in children and adults
According to the World Health Organization diagnostic classification, AO (in postmenopausal females and males ≥50 years of age) is defined based on BMD at the hip or lumbar spine that is ≤2.5 standard deviations (SDs) below the mean BMD of a young adult reference population (T score) [12]. However, PO is not based on densitometry findings. Consequently, the definition presented in 2013 was supported in 2019 [3]. PO is defined by the presence of one or more vertebral compression (crush) fractures in the absence of local disease or high-energy trauma, or in the presence of BMD z-score ≤ -2.0 SD associated with fracture history, 2 or more long bone fractures by the age of 10 years, or 3 or more long bone fractures at any age up to 19 years. Furthermore, in children <18 years of age, the z-score should be used rather than T score.
The association between low bone mass and fractures is less well defined in children, and the reference database to generate z-scores is limited compared with the reference database in adults. The term "low bone density for chronologic age" is preferred if z-scores are ≤-2.0 based on pediatric databases of age-matched controls. Therefore, since the 2013 ISCD Official Positions, vertebral fracture (VF), which is a loss of vertebral height ratio >20% according to the Genant semiquantitative method, was identified as an osteoporotic event even in the absence of low bone density [3,4]. Furthermore, according to the 2019 ISCD Official Positions, PO is diagnosed in the presence of VF even in the absence of low BMD [3]. The distinction in the definition of PO, particularly the inclusion of fractures as a diagnostic criterion, highlights a significant contrast between this condition and AO [13]. The high incidence of fractures between birth and 16 years of age is a recurring finding in almost all epidemiological studies. The possibility of a nonclinically significant fracture in a child led the ISCD 2013 Official Positions Statement to define a threshold number of long bone fractures, which was supported in the 2019 meeting [14,15].
Osteoporosis assessment
Although quantitative computed tomography (QCT), peripheral QCT (pQCT), and high-resolution pQCT (HR-pQCT) are the primary research techniques used for 3-dimensional evaluation of bone microarchitecture parameters, dual-energy x-ray absorptiometry (DXA) remains the gold standard method for quantitative assessment of the bone in adults and children [3,4]. However, in children, key differences in the performance and interpretation of results should be considered.
1. Measurement sites
The densitometry examination of adults needs to include at least 2 sites, typically the lumbar spine and proximal femur. However, the ISCD 2019 Official Positions on this matter is clear: whenever technically feasible, the posterior-anterior spine and bodyless head (TBLH) are the preferred sites and should be measured to help with diagnosis and monitoring.
Three measurement sites have been added and listed in the 2019 ISCD: proximal femur, lateral distal femur, and 1/3 radius. Proximal femur DXA measurement is particularly important in children with a reduced mechanical load on the lower extremities and for densitometry monitoring during the transition to adulthood. However, the measurement should be interpreted with caution especially before the age of 15 years due to the presence of ossification nuclei. The fusion of cephalic and trochanteric ossification nuclei occurs between the ages of 13 and 15 years. DXA measurements in the lateral distal femur and 1/3 radius are usually recommended when evaluating other standard skeletal sites is difficult. This may be the case in children with orthopedic hardware, severe scoliosis, other skeletal deformities, or who cannot stand or have difficulty standing. In addition, adequate reference data must be available for all discussed sites. The same principle applies to adults (per the 2019 ISCD Official Positions). The forearm BMD (1/3 radius) should be measured if the hip and/or spine cannot be measured or interpreted, the patient has hyperparathyroidism, or is very obese (over the weight limit for the DXA table).
For DXA follow-up, using the same device, same acquisition methods, and software is important [16].
2. Reference data
The most limiting factor in BMD studies and interpretation of DXA scores in children is likely the lack of reference baseline data. Establishing a reference population of similar gender, age, and ethnic origin is necessary before considering using the z-score. Although DXA is a technique with very minimal radiation, performing densitometry examinations in healthy children generates ethical concerns. Although some normative BMD values for the lumbar spine and femoral neck [17,18]. TBLH [19,20], and distal forearm [21] exist, reference data are still considered scarce in the pediatric population, and further studies are required. In adults, The ISCD recommends using a young Caucasian female normative database for females and males of all ethnic groups [22].
3. Disadvantages of DXA interpretations in children and adolescents
DXA should be cautiously interpreted, taking into consideration all potential factors that could either falsely elevate or diminish bone density [23]. Scholz et al. [24] identified potential sources of error and risks in the interpretation of bone densitometry. In a study on the prevalence of DXA interpretation errors, technical errors were identified in 90% of patients and 42% were major errors (defined as incorrect information that could potentially lead to inappropriate care decisions for the patient) [25]. However, the interindividual variability of height and weight growth, pubertal status, and bone age must be determined and taken into consideration [26]. Because DXA measures BMD in a 2-dimensional image, volumetric BMD (g/cm3) is underestimated in short-stature children and overestimated in tall children. Errors in DXA measurements are also common in adults and can be categorized as patient positioning, data analysis, artifacts, and/or demographics [24].
4. VF assessment
VFs are indicative of bone fragility and may be present without BMD loss. However, VFs have been underestimated because the majority are clinically silent. Vertebral assessment fracture (VFA) was proposed in adults and pediatrics as a lowradiation technique to screen VFs.
VFA is preferred to spine imaging to detect symptomatic and asymptomatic VFs. The method of choice is The Genant visual semiquantitative method [3]. In addition, the 2019 ISCD recommendations identified situations in which further spine imaging should be considered in children: insufficiently visible vertebrae if confirmation of a VF would affect clinical and therapeutic management and signs of nonosteoporotic fracture (inflammatory, infectious, or malignant origins). However, in adults, VFA or spine imaging is indicated when the T score is < -1.0 and associated with height loss or glucocorticoid therapy or advanced age (females 70 years of age or males 80 years of age).
5. When bone densitometry should be considered
Etiologies of PO overlap with AO. However, some specificities should be recognized, mainly regarding primary osteoporosis. For example, primary osteoporosis in children comprises a broad range of skeletal and extraskeletal conditions, from mild to lethal. Genotypic osteoporosis constitutes the larger portion of PO [27]. Osteogenesis imperfecta is the most common, affecting 1/15,000–20,000 children a year. Secondary osteoporosis encompasses different causes of acquired bone fragility and is the consequence of immobility or muscle impairment, inflammatory conditions with increased cytokine levels (e.g., chronic arthritis, malignancies, inflammatory bowel diseases, autoinflammatory diseases), long-term steroid use and other medication use, several endocrinopathies, and some gastrointestinal disorders resulting in malabsorption syndromes.
The classic situations in which DXA is recommended are children "with primary bone disease, or at risk for a secondary bone disease" (ISCD 2019). Repeated fractures and/or for moderate trauma and certain chronic diseases including endocrinopathies, in particular, hypogonadism and hypercorticism, pubertal delays, long-term corticosteroid therapy, chronic inflammatory diseases, chronic nephropathy, immobilization, and malnutrition were discussed as potential situations [28,29]. Galindo-Zavala et al. [29] recommended following the existing guidelines for each pathology because universal consensus on BMD monitoring in children is not available. In adults, DXA should be performed for the following: females ≥65 years of age and males ≥70 years of age; postmenopausal females and males 50–69 years of age; based on risk profile; postmenopausal females and males ≥50 years of age with a history of adult-age fracture [22].
Medical approach
A unanimous principle that applies to both AO and PO is that management of secondary osteoporosis starts with management of the underlying disease. General management is integral to bone health and should be considered for all ages.
1. General measures
Supplementation with vitamin D and calcium is also a pragmatic approach and highly recommended in children and adults at risk of bone fragility. According to the review of Beck et al. [30] that included 85 papers on pediatric bone health, vitamin D deficiency correlated with lower bone density, increased fracture risk, low back pain, skeletal deformities, and poorer bone surgery outcomes.
Current recommendations for calcium intake are 500 mg per day for children 1–3 years of age, 800 mg for children 4–8 years of age, and 1,300 mg for children 9–18 years of age [30]. However, the Bone Health and Osteoporosis Foundation proposed a dose of 1,000 mg/day of calcium for males 19–70 years of age and females 19–50 years of age, and 1,200 mg/day for females ≥51 years of age and males ≥71 years of age [22]. Similarly, the American College of Rheumatology has recently updated its 2017 guidelines on glucocorticoid-induced osteoporosis in children and adults recommending that all children treated with glucocorticoids at any dose for >3 months should be supplemented with vitamin D and calcium and their diet optimized [31].
Regarding serum 25-hydroxyvitamin D concentration, some authors suggest levels >30 ng/mL in patients with higher fracture risk [29,32]. Addressing socioeconomic and demographic disparities when feasible, as well as encouraging healthier lifestyles with weight-bearing activities are also important general measures [30,33-35].
2. Bisphosphonates
Bisphosphonate (BP) is a pyrophosphate-derived agent that inhibits osteoclastic function and is the most widely used drug for the treatment of osteoporosis. BPs improve bone mass and strength by reducing bone resorption and sustaining bone formation. BPs are considered at initial pharmacologic treatment in postmenopausal females and males ≥50 years of age who have a severe fracture or low bone density with risk factors for fracture [36]. However, their indications in children are challenging because they are off-label worldwide in the pediatric population.
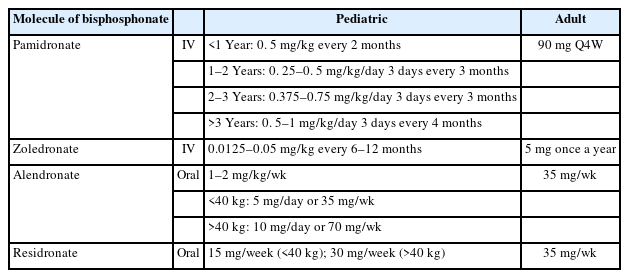
Treatment with BPs is the standard approach in children, although no formal consensus has been reached on the molecule, dose, or duration. The molecule choice differs for adults and children; pamidronate is preferred in children, but its usefulness in postmenopausal osteoporosis remains controversial. The proposed dose of BPs in children and adults is summarized in Table 1.
Regarding the mode of administration, a systematic Cochrane review on BPs in children showed that oral and intravenous administration resulted in similar increases in BMD [37]. In children with less potential for vertebral body reshaping (children administered steroids for >3 months, sub-normal mobility, poorly controlled underlying disease, older age with less residual growth potential, and severe collapse) BP therapy is indicated [38]. Pamidronate 4.5–9 mg/kg body mass/yr, divided into 3 treatment cycles (1 cycle every 4 months), and zoledronic acid 0.05–0.1 mg/kg body mass/yr, divided into 2 treatment cycles (1 cycle every 6 months) are the preferred drugs [38].
Conversely, there is more potential for spontaneous vertebral body reshaping in the presence of transient risk factors (<3 months of steroids, immobilization <2 weeks, well-controlled underlying disease), younger age (≥8 years of age in girls and 9 years in boys), and milder collapse [38]. In such a clinical scenario, the general practice is to continue monitoring with repeating DXA after 6–12 months [38].
Oral and intravenous BPs are conditionally recommended only in children with an osteoporotic fracture who are continuing treatment with glucocorticoids at a dose ≥0.1 mg/kg/day for >3 months because they are considered at high risk of recurrent fracture [31].
In the United States recommendations regarding the diagnosis and treatment of secondary osteoporosis in children [29], the bone remodeling ability was not taken into account. The consensus was that children fulfilling the osteoporosis criteria (z-score ≤-2 and pathological fracture or VF irrespective of z-score) should be started on treatment with BPs. The panel also agreed that patients without osteoporosis but who have not reached the desirable bone mass and have a low BMD in early puberty (Tanner II) can also be started on BPs under the following conditions: presence of active risk factors z-score ≤-2.5 SD and a declining BMD on 2 separate DXAs 1 year apart; patients without active risk factors but with z-score ≤-3 SD and a declining BMD on two separate DXAs 1 year apart [29]. To date, an official scientific society has not validated these recommendations.
Most children with secondary osteoporosis recover well without treatment with BPs. Aggressive treatment is considered for older children, those with severe spinal collapse and persistent risk factors [29].
Based on these findings, further studies are needed and multidisciplinary decision-making should include the patient and/or the parents when managing osteoporosis.
The safety profile of BPs is favorable in both children and adults. Similar to adults, intravenous BP can induce an acute phase reaction with fever, bone pain, and myalgia that can be resolved with paracetamol and fluids. Oral administration of BPs, especially zoledronic acid, may cause gastrointestinal side effects [39]. However, gastrointestinal effects in children appear to be an uncommon finding in pediatric studies. Concerns have been raised regarding the risk of osteonecrosis of the jaw associated with BP therapy. Fortunately, this complication is very rare in adult osteoporotic patients and no reports of osteonecrosis of the jaw were described in childhood [40,41].
Another issue that has limited the use of BPs in females was the ability of the drug to cross the placenta and disturb fetal skeletal formation [42]. However, a case-control study in which females with systemic or bone diseases and who had taken BPs in the 6 weeks before or during pregnancy were compared with females not exposed to BPs or any teratogenic agent, major teratogenic effects due to BPs were not observed [43]. In other reviews, published data on maternal use of BPs and its outcomes on fetuses and newborns were evaluated; BPs before or during pregnancy were not associated with serious fetal or neonatal side effects [44-46]. However, due to some case reports of congenital malformations in pregnant women treated with BPs, the use of BPs during pregnancy is generally avoided and caution with their use in fertile women is recommended [47].
DXA should be performed 1–2 years after initiating or changing treatment or when considering drug holidays [22]. The interval between 2 DXA scans differs between children and adults. According to the ISCD Official Positions, DXA can be repeated after a minimum of 6–12 months in children and in adults at an interval of 1–2 years due to low bone turnover.
Denosumab is another potent inhibitor of bone resorption and has been studied among adults in the randomized FREEDOM trial [48]. The reversible effect on bone turnover after discontinuation of denosumab represents the key difference with BPs. However, beneficial effects on bone turnover, bone density, and some bone tumors have been reported with denosumab [49].
Anabolic therapy (growth hormone, androgens, teriparatide) appears an attractive option for PO patients with low bone turnover such as neuromuscular disorders and glucocorticoidinduced osteoporosis [50,51]. However, contrary to adults, data on its potential efficacy and safety for children with osteoporosis are not available.
Conclusion
In conclusion, understanding changes in bone health throughout life is important. Although bone health in adults is closely intertwined with that of children, notable distinctions exist. In adults, osteoporosis is defined based on densitometry measurements, and in children the diagnosis is focused on bone fragility and fractures. DXA is the gold standard for assessing bone health in both children and adults but requires adjustment for bone or skeletal size. Although BPs are the drug of choice for the treatment of AO, their use remains challenging in the pediatric population.
Furthermore, vertebral reshaping and remodeling reflect the uniqueness of the pediatric bone and explain why background antiresorptive treatment is not always indicated, unlike in adults.
Although the relationship between BMD and fracture risk in adults has been well documented, further studies are required to better understand the association in children.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author contribution
Conceptualization: HLF; Data curation: HLF; Methodology: KM; Project administration: HLF; Visualization: DBN; Writing - original draft: IC; Writing - review & editing: DK, WH