2. Parks JS. Gene sequence and production. of recombinant MetGH/hGH. Pediatr Endocrinol Rev 2018;16(Suppl 1):17–27.
3. Long Island University, Clinical Drug Experience Knowledgebase: Kabi Pharmacia [Internet]. Brookville (NY): Long Island University; 2003 [2022 Sep 1]. Available from:
https://www.cdek.liu.edu/org/1112/.
4. Wallström A, Trulsson L. The Kabi International Growth Study: rationale, organization, and development. In: Ranke MB, Gunnarsson R, editors. Progress in growth hormone therapy – 5 years of KIGS. Mannheim (Germany): J&J Verlag, 1994;1-9.
5. Wilton P. KIGS: structure and organization. Growth hormone therapy in pediatrics. 20 years of KIGS. In: Ranke MB, Price DA, Reiter EO, editors. Basel (Switzerland): Karger, 2007:1-5.
6. Non-interventional study abstract for external disclosure. Protocol A6281306 (87-052). KIGS® (Pfizer International Growth Database). New York (NY): Pfizer; 2014.
7. Ranke MB. The KIGS aetiology classification system. Progress in growth hormone therapy – 5 years of KIGS. In: Ranke MB, Gunnarsson R, editors. Mannheim (Germany): J&J Verlag, 1994:51-61.
8. Wilton P. Adverse events during growth hormone treatment: 5 years' experience in the Kabi International Growth Study. In: Ranke MB, Gunnarsson R, editors. Progress in growth hormone therapy – 5 years of KIGS. Mannheim (Germany): J&J Verlag, 1994:291-307.
10. Ranke MB. Who stops growth hormone in KIGS - and why? Growth hormone therapy in pediatrics. 20 Years of KIGS. In: Ranke MB, Price DA, Reiter EO, editors. Basel (Switzerland): Karger, 2007:183-8.
11. Gutiérrez LP, Kołtowska-Häggström M, Jönsson PJ, Mattsson AF, Svensson D, Westberg B, et al. Registries as a tool in evidence-based medicine: example of KIMS (Pfizer International Metabolic Database). Pharmacoepidemiol Drug Saf 2008;17:90–102.


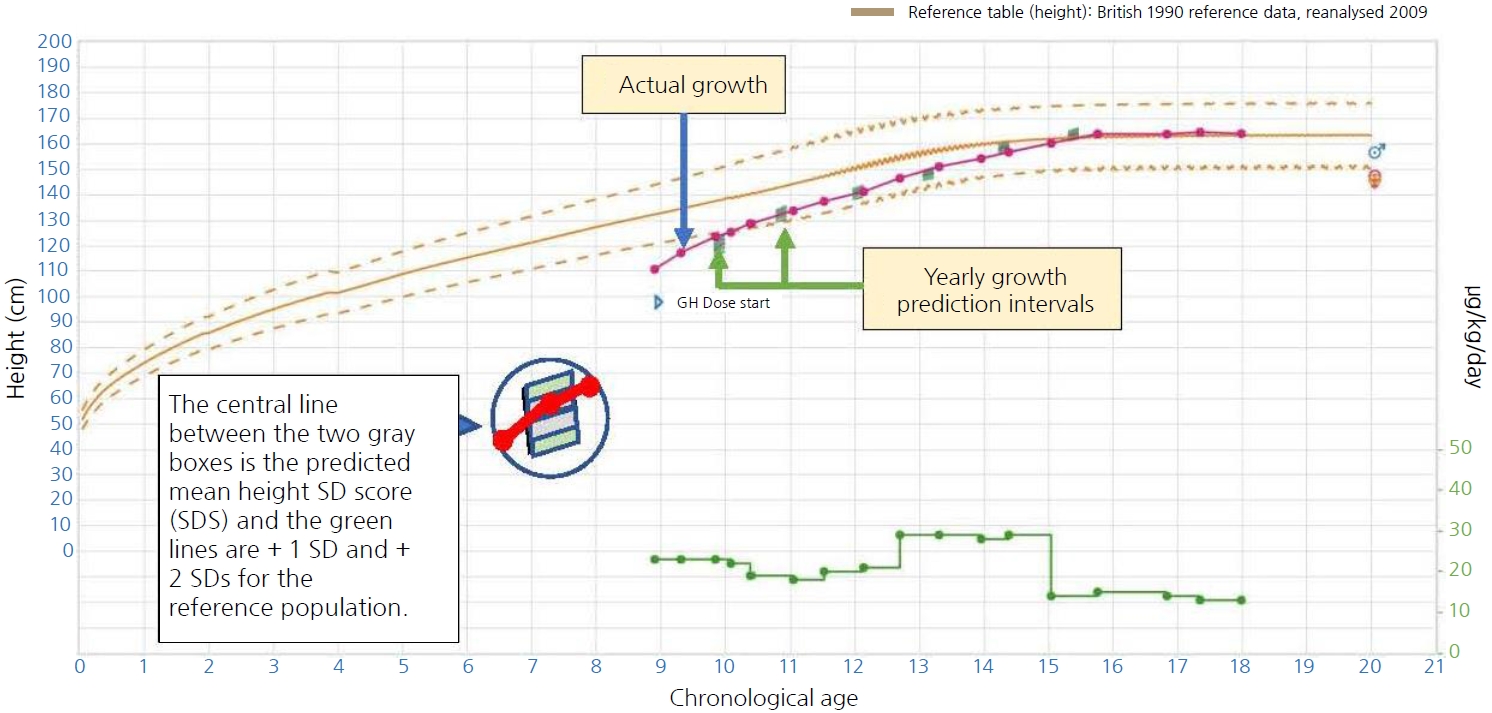
13. Ranke MB, Lindberg A. Predicting growth in response to growth hormone treatment. Growth Horm IGF Res 2009;19:1–11.


14. Ranke MB, Lindberg A. Predicting growth in response to growth hormone treatment – the KIGS approach. Growth hormone therapy in pediatrics. 20 Years of KIGS. In: Ranke MB, Price DA, Reiter EO, editors. Basel (Switzerland): Karger, 2007:422-31.
16. Loftus J, Lindberg A, Aydin F, Gomez R, Maghnie M, Rooman R, et al. Individualised growth response optimisation (iGRO) tool: an accessible and easy-to-use growth prediction system to enable treatment optimisation for children treated with growth hormone. J Pediatr Endocrinol Metab 2017;30:1019–26.


18. Verhelst J, Kendall-Taylor P, Erfurth EM, Price DA, Geffner M, Koltowska-Häggström M, et al. Baseline characteristics and response to 2 years of growth hormone (GH) replacement of hypopituitary patients with GH deficiency due to adult-onset craniopharyngioma in comparison with patients with nonfunctioning pituitary adenoma: data from KIMS (Pfizer International Metabolic Database). J Clin Endocrinol Metab 2005;90:4636–43.


19. Yuen KC, Koltowska-Häggström M, Cook DM, Fox JL, Jönsson PJ, Geffner ME, et al. Clinical characteristics and effects of GH replacement therapy in adults with childhood-onset craniopharyngioma compared with those in adults with other causes of childhood-onset hypothalamic-pituitary dysfunction. Eur J Endocrinol 2013;169:511–9.


21. Yuen KCJ, Mattsson AF, Burman P, Erfurth EM, Camacho-Hubner C, Fox JL, et al. Relative risks of contributing factors to morbidity and mortality in adults with craniopharyngioma on growth hormone replacement. J Clin Endocrinol Metab 2018;103:768–77.


22. Darendeliler F. Growth hormone treatment in rare disorders: the KIGS experience. 20 Years of KIGS. In: Ranke MB, Price DA, Reiter EO, editors. Basel (Switzerland): Karger, 2007:213-39.
23. Ranke MB, Gunnarsson R, editors. Progress in growth hormone therapy – 5 years of KIGS. Mannheim (Germany): J&J Verlag, 1994:1-313.
24. Ranke MB, Wilton P, editors. Growth hormone therapy in KIGS – 10 years experience. Leipzig (Germany): Johann Ambrosius Barth Verlag, 1999:1-409.
25. Ranke MB, Price DA, Reiter EO, editors. Growth hormone therapy in pediatrics – 20 years of KIGS. Basel (Switzerland): Karger, 2007;1-511.